Strokes, or brain attacks, are a leading cause of death in America (pdf). In 2020, stroke caused 1 out of 21 deaths (pdf) in the United States. Luckily, many who survive a stroke can recover with minimal complications. Rehabilitation and lifestyle changes can improve recovery and minimize the risk of recurrence.
A stroke is a medical emergency caused by a loss of oxygen to the brain. Within minutes, brain cells die, which can result in lifelong complications or even death.
Recognizing the symptoms or signs of a stroke quickly will improve the chances of successful recovery.
What Are the Common Types of Stroke?
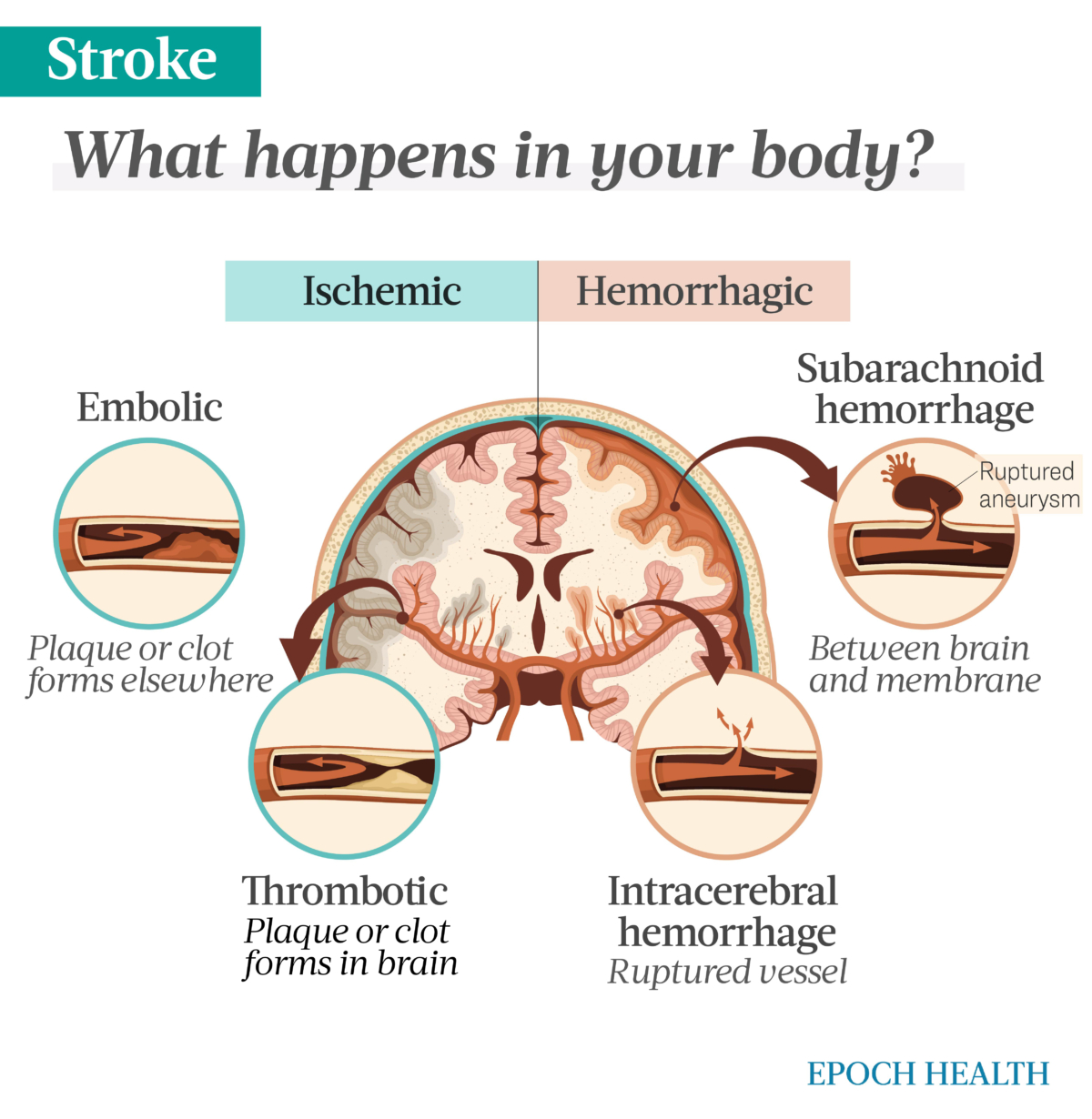
There are two common types of stroke, each with two subtypes. What causes the interruption of oxygen and blood flow to the brain is what differentiates them. The following are the two main types of stroke and their subtypes:
Ischemic
Hemorrhagic
Intracerebral
Subarachnoid
What Are the Symptoms and Early Signs of Stroke?
Quickly recognizing the signs or symptoms of stroke can significantly improve the stroke patient’s outcomes. A simple acronym to help remember the signs and symptoms of stroke is F.A.S.T.:
Face drooping: Facial muscles appear slack or droop
Arm weakness: Numbness or weakness in the arms, legs, or face, especially on one side of the body
Speech difficulty: Slurred words and confusion in understanding or speaking
Time to call 9-1-1
Less frequent symptoms can include:
Visual disturbances: Difficulty seeing out of one or both eyes
Headache: Sudden, severe headache without a known cause
Loss of mobility: Loss of balance or coordination
Disorientation
Memory loss
What Causes a Stroke?
A stroke’s cause depends on its type. Ischemic strokes are caused by blockage, while hemorrhagic strokes are caused by a leaking or burst blood vessel or ruptured aneurysm.
Blocked Artery (Ischemic)
An ischemic stroke is the most common type, with approximately 87 percent of all strokes being ischemic. Ischemic strokes are caused by blockage.
An artery can become blocked in multiple ways. A buildup of fatty deposits (plaque) or a blood clot can block a vessel.
A transient ischemic attack (TIA) is a temporary disruption of blood flow to the brain. The interruption resolves within minutes and usually does not result in permanent complications. These are sometimes referred to as ministrokes.
Leaky or Burst Blood Vessel (Hemorrhagic)
Leaking or burst blood vessels can cause a hemorrhagic stroke. Several factors can contribute to this:
Uncontrolled high blood pressure
Blood thinners (anticoagulants)
Bulges in weakened blood vessel walls (aneurysms)
Trauma
Protein deposits in blood vessel walls resulting in weak vessel walls (cerebral amyloid angiopathy)
Ischemic stroke
Irregularities in the brain’s vasculature (arteriovenous malformation)
When blood leaks or bursts from the blood vessel, it puts pressure on brain tissue. This pressure damages brain cells, leading to hemorrhagic stroke.
What Are the Mechanisms Behind Stroke?
A few mechanisms are behind the primary causes of stroke: blockage (ischemic) or a leaky or burst vessel (hemorrhagic). The mechanisms are detailed below.
1. Ischemic Stroke
The buildup of plaque in the arteries can become hard, causing atherosclerosis. As hardening plaque collects in the vessel, passage through the vessels narrows, limiting blood flow.
The plaque building up on the artery wall can break. Platelets in the blood can then stick to the damaged area of the plaque and form a clot. The clot can partially or fully block the artery. According to the National Institute on Neurological Disorders and Stroke, this is the most common way arteries become blocked. Inflammation may also cause artery blockage by promoting plaque accumulation.
Ischemic strokes are divided into two types:
Thrombotic: Thrombotic strokes occur when plaque buildup causes blood proteins to accumulate into a complete blockage, called a thrombus. The plaque or clot can travel to the brain from elsewhere in the body, but the blockage occurs in the brain.
Embolic: Embolic strokes result from a clot that has developed elsewhere in the body that disrupts blood flow to the brain. An artery may become blocked by a traveling blood clot from the left side of the heart or the carotid arteries or by debris (for example, from an infected heart valve). Untreated atrial fibrillation, a common arrhythmia of the heart, is a risk factor for emboli to the brain.
2. Hemorrhagic Stroke
A hemorrhagic stroke is when a blood vessel in the brain leaks or bursts. As pressure builds within the brain from the bleeding, cells become damaged. As their access to oxygen further declines, they begin to die.
Hemorrhagic strokes account for about 13 percent of all strokes. This type is further divided into two categories:
Intracerebral: An intracerebral hemorrhage results from bleeding into the main tissue of the brain. This type of bleeding may also be called parenchymal hemorrhage.
An intracerebral hemorrhage occurs swiftly and without warning. These strokes can be severe and lead to coma or death.
Subarachnoid: With subarachnoid hemorrhaging, the bleeding happens in the space between the brain and its surrounding membrane. This space is called the subarachnoid space.
An aneurysm can cause bleeding in this space. An aneurysm is a bulge in a weakened part of the blood vessel wall.
Ischemic strokes are caused by blockage, and hemorrhagic are caused by a leaking or burst blood vessel. (The Epoch Times)
Who Is More Likely to Have a Stroke?
Many factors can put a person at risk for stroke. Some factors can be controlled by lifestyle, while others cannot. The following factors increase a person’s risk for stroke:
Family history of stroke
COVID-19 infection
Diabetes
Cardiovascular disease
Obstructive sleep apnea
Previous TIA: Though they are called ministrokes, transient ischemic attacks (TIA) are as significant as any other stroke and indicate future strokes. Over one-third of people who have had an untreated TIA have a stroke within one year, and 10 to 15 percent have a stroke within three months.
Age: Older people are more likely to have strokes than younger.
Race or ethnicity: Blacks and Hispanics, especially males, are likelier to have strokes than other ethnic groups. These groups tend to have more cases of high blood pressure, diabetes, obesity, and tobacco smoking. Blacks also are most susceptible to the genetic disorder sickle cell disease, which increases stroke risk.
Sex: Men are more at risk than women because, according to the U.S. Centers for Disease Control and Prevention (CDC), half of them have high blood pressure, and they are more likely to drink alcohol and smoke than women. Approximately 3 in 4 are overweight or obese, and they are more likely to have diabetes and less likely to get enough physical activity. The CDC also claims men under 44 are hospitalized more frequently than women in the same age group for certain types of strokes.
Obesity: Obesity contributes to high blood pressure, heart disease, and diabetes, all risk factors for stroke.
Poor sleep habits: Studies have shown that both people who get too much sleep and too little sleep are at higher risk of stroke. People who have had a stroke may also have sleep disturbances, which can put them at risk for recurrent strokes.
Traumatic brain injury (TBI): TBIs can increase the risk of stroke. The trauma may cause bleeding in the brain, causing damage similar to that of a hemorrhagic stroke. Neck injuries can also increase the risk of stroke, especially in young adults.
Previous stroke: The risk of a recurrent stroke is higher soon after a stroke but decreases with time. According to Johns Hopkins, approximately 3 percent of people who’ve had a stroke have another within 30 days, while 33 percent have another within two years.
Women
Some studies find that women may experience more severe strokes and are more likely to die from them, as they tend to have strokes at an older age. They also have unique risk factors, such as pregnancy, childbirth, and menopause. Contributing risk factors during pregnancy are:
Increase in blood clotting proteins
Preeclampsia (high blood pressure with fluid retention)
Infection
Postpartum drop in blood volume or rapid hormonal change
Age
The risk of stroke is higher in adults over 55 and increases with age. Older people have a higher prevalence of ischemic stroke, which may be due to higher cholesterol levels, diabetes, or atherosclerosis.
According to the National Institute on Neurological Disorders and Stroke, children are at the highest risk of stroke during the perinatal stage of pregnancy. This period is before birth and a couple of weeks after. Children are often vulnerable at this stage due to congenital heart problems or head trauma. Generally, black children are at a higher risk, typically because sickle cell anemia (a sickle cell disease) is a high stroke risk.
The symptoms of stroke in children are similar to those in adults. Children may have a headache and paralysis or weakness on one side of the body. Other symptoms may include seizures, difficulty breathing, and loss of consciousness.
For children, the outcomes are worse than those of adults if the stroke occurs when the child is younger than 1 year old and if they lose consciousness during the stroke, regardless of age. However, children who have a stroke generally fare better than adults in rehabilitation due to the brain’s ability to adapt and rewire.
Other Factors
Socioeconomic factors have also been shown to affect the risk of stroke. Strokes are more common among those with a lower income. One reason may be the links between smoking and obesity, which occur more often in lower-income populations. Another explanation may be the population’s more limited access to health care.
People with other conditions, including the following, are also more at risk:
While there are several risk factors that a person can’t modify, many more can be modified, including:
Lack of physical activity
Heavy alcohol use
Tobacco use
Illegal drug use, particularly cocaine and methamphetamines
High blood pressure
High cholesterol
Birth control use
How Is a Stroke Diagnosed?
Symptoms alone can’t determine if you have had a stroke. Once you arrive at the hospital, a medical team will conduct tests to determine if you had a stroke, TIA, or other medical event.
Health care providers will initially do a neurological exam with a questionnaire and physical tests. Providers will then use a scale to assess stroke severity. Typically, this is the standardized NIH Stroke Scale.
Other scales, such as Glasgow Coma Scale and the Modified Rankin Scale, may also be used. These types of scales help to measure the stroke’s resulting disabilities.
Health care providers may use other tests, such as:
Computed tomography (CT) scan: A brain scan primarily rules out bleeding. After three hours, it may identify damaged tissue if it covers a large area.
Diffusion-weighted imaging (DWI): This type of MRI measures the movement of water in the brain and can detect ischemic stroke before non-contrast CT.
Catheter-based angiography: This determines the extent of blockages in blood vessels.
Ultrasound: This test checks for atherosclerosis in the carotid artery.
Doppler ultrasound: This measures blood velocity in large blood vessels.
Cardiac ultrasound: This type of ultrasound identifies clots in the heart that may break loose.
Blood tests: Blood tests can check for blood clotting.
Holter monitor: This device is worn for several days to get an electrocardiogram (EKG) measurement and check for atrial fibrillation.
Lumbar puncture: A “spinal tap” extracts fluid from the spinal canal to help identify hemorrhagic stroke that is initially too small to see on a CT scan (but still suspected due to excruciating new headache).
Echocardiogram: This test uses sound waves to identify clots in the heart that may have migrated to the brain.
Cerebral angiogram: Though uncommon, this X-ray test gives doctors a view of a person’s neck and head arteries.
What Are the Complications of Stroke?
There are many possible complications of stroke. The severity and duration depend on where the stroke occurred and how long the brain was without oxygen.
The more common complications of stroke are:
Paralysis, typically on one side of the body.
Difficulty swallowing (dysphagia) due to weakened throat muscles.
Speech and language problems usually due to damage on the left side of the brain.
Memory loss.
Cognitive deficits like difficulty thinking or understanding concepts.
Emotional problems like difficulty controlling one’s emotions or depression.
Pain and numbness normally on the affected side.
Behavioral changes.
Difficulty performing self-care.
Each area of the brain is responsible for different bodily functions. Because of this, the stroke’s origin determines what complications a person will have. It also determines the severity and duration of those complications, which may be permanent or temporary.
The following are other complications that may be less common:
“Neglect” syndrome: People experiencing this syndrome are unaware of one side of their body. The person may have no field of vision on that side or may be unaware of problems on that side.
Vascular cognitive impairment: Vascular cognitive impairment (VCI) is a permanent decline in cognitive function.
Central pain syndrome: This type of pain is a mixture of sensations. The person could feel hot, cold, tingling, numbness, or sharp stabbing, to name a few. Damage to the brain’s thalamus, which is involved in sensory perception, is the culprit. This pain will be intense in the area of the body affected by the stroke and is made worse with movement and changes in temperature.
Increased pressure on the brain: Sometimes, ischemic stroke can cause swelling, putting pressure on the brain. Increased pressure can be life-threatening.
Post-stroke seizures: Seizures occur in 5 to 9 percent of all people who have had a stroke. These are more common in hemorrhagic strokes and occur within the first year of the stroke.
Urinary complications: After having experienced a stroke, people may have what is called a neurogenic bladder. A neurogenic bladder can cause increased or decreased urinary frequency, urgency, incontinence, or incomplete emptying of the bladder.
Fecal complications: People who have experienced a stroke may acquire fecal incontinence, which is the inability to control when and where a person defecates. Older patients and women are more at risk of developing this complication.
Vascular dementia: This type of dementia is the second most common cause of dementia after Alzheimer’s disease.
Spasticity and contracture: Strokes may cause involuntary muscle activity called spasticity, resulting in muscle stiffness. Contractures are deformities that cause muscles and joints to shorten or tighten and can result in pressure sores.
Hemiplegic shoulder pain: Hemiplegic shoulder pain (HSP) typically occurs two to three months after a stroke. There are four types: misaligned joint, spastic muscle, diffuse pain, and reflex sympathetic dystrophy. The pain can remain in the shoulder or radiate down the arm.
Emotional lability: When a person who has had a stroke cries excessively or laughs at nothing seemingly funny, they are experiencing emotional lability. This condition can also be called pseudobulbar affect. The condition occurs without the presence of depression.
Depression: Depression following a stroke can be a serious problem. If left untreated, it can slow the progression of rehabilitation or may lead to suicide in extreme cases.
What Are the Treatments for Stroke?
Treatments for stroke depend on its type. For ischemic strokes, treatment includes medications that will break up clots, procedures to remove clots, and restoration of blood flow to the brain. Treatments for hemorrhagic strokes involve procedures to stop a leaking blood vessel or repair a burst vessel, such as surgical clipping and coiling of the vessel.
Ischemic
Drug therapy is the most common treatment for early ischemic stroke. Clot-busting medications can be very effective when treating ischemic stroke. The caveat is that they have to be given soon after the signs or symptoms of a stroke begin.
For this reason, it is essential to note the time a stroke occurs. Medications that break up clots—thrombolytic drugs—need to be given within three hours of the onset of symptoms to be effective and are given intravenously. These types of drugs can significantly improve a person’s chance for a faster recovery.
Restoring blood flow to the brain as quickly as possible during an ischemic stroke can mitigate damage caused by the lack of oxygen to the brain. When oxygen returns, cells stop dying, and tissue that wasn’t damaged remains unharmed.
Medications are not the only way to restore blood flow to the brain when a vessel is blocked. A physician may opt to remove the clot with a stent retriever. A catheter is run through the blood vessel to the clot and retrieves it. This procedure may be used in conjunction with medication.
Hemorrhagic
Before a vessel can be fixed or a leak can be stopped, the troubled vessel has to be located. Once a physician locates the bleeding, he or she performs one of two procedures: clipping or coiling.
Clipping is one way to treat brain aneurysms before they burst. These weak areas of vessels can expand like a balloon that may eventually burst. In this case, the aneurysm will have sprung a leak.
A neurosurgeon will then perform the clipping procedure. A clamp is put on the neck of the aneurysm to prevent it from bursting. Patients must be closely monitored after this procedure.
The other option is a coiling technique called endovascular embolization. Endovascular embolization is used for more high-risk cerebral aneurysms. A coil is placed in the aneurysm, triggering an immune response from the body. This results in the formation of clots on the wall of the aneurysm, which restores some strength to those weakened walls.
Should there be a case where neither procedure repairs the aneurysm, it may be necessary to occlude (close) the vessel. This stops blood flow to the vessel before it reaches the area of the aneurysm. No longer having blood flow to the aneurysm removes the risk of leak or rupture.
While these are ways to address the stroke itself, they do not address the consequences of a stroke. Recovery from the physical consequences of a stroke calls for rehabilitation.
Rehabilitation
Rehabilitation is essential to recovering from a stroke’s physical and mental complications. Rehabilitation can include:
Physical therapy: Helps the patient relearn activities such as walking, standing, sitting, and transferring positions and avoid muscle contractures and skin sores
Occupational therapy: Helps the patient relearn daily activities like eating and drinking
Speech therapy: Helps the patient relearn how to talk and understand language
Vocational therapy: Helps the patient return to work
Psychological therapy: Assists with depression, anxiety, frustration, and anger. Family members may also benefit from this type of therapy.
Rehabilitation will begin as soon as possible. During the first few days of rehabilitation, sessions can be as often as hourly. While the patient remains in the hospital, sessions can be up to six times daily. When out of the hospital, rehabilitation can occur in an inpatient rehabilitation facility, where a patient will remain until rehabilitation is complete.
Rehabilitation Systems
Some newer treatments are the Neurolutions Upper Extremity Rehabilitation System and the MicroTransponder Vivistim Paired VNS (vagus nerve stimulation) System.
The Neurolutions Upper Extremity Rehabilitation System is available to people 18 years and older with a disability of the upper arm due to a stroke. This system requires the person to wear a hand brace. The hand brace works with a table and electrodes that record brain activity and tell the brace to move the hand.
The MicroTransponder Vivistim Paired VNS System is used along with stroke rehabilitation for persons with upper extremity impairment due to chronic ischemic stroke. This system stimulates the vagus nerve in an effort to improve the motor function of the upper extremities.
How Does Mindset Affect Stroke?
A person’s outlook on life and how they perceive their rehabilitation can help prevent a stroke and help when rehabilitating from one.
Studies have shown that optimistic people have a lower risk of death from stroke. Optimistic people also tend to have better coping abilities than pessimistic people.
Negative emotions create a physical stress response and release hormones that can increase the heart rate and blood pressure, risk factors for stroke. People with a negative outlook may end up coping by self-medicating and may use other substances that can also increase the risk factor of stroke.
Mental illness can increase the prevalence of stroke risk factors as well. People with mental illness are more likely to smoke, be obese, and have high blood pressure and diabetes.
Adults with mental illness are also more likely to have cardiovascular disease, increasing stroke risk. This risk can increase over time.
What Are the Natural Approaches to Stroke?
There are many complementary and alternative treatments and prevention methods for stroke—from newer techniques to the more traditional approaches in holistic practices.
Behavioral changes can minimize many stroke risk factors, yet motivating people to make those changes can be challenging. Fortunately, the emergence of technologies such as digital phenotyping, social network analysis, machine learning, and gamification may be able to facilitate existing behavioral interventions. Encouragement and motivation can reinforce positive behaviors and modify negative behaviors, resulting in behavior modification.
“Gamification” uses game participation to reinforce good behaviors. For example, employers could introduce a weight-loss challenge to employees that drives positive behaviors, increasing participants’ likeliness of winning the game. Social media and other technologies, such as text messaging, can provide reminders and social connections to encourage positive behaviors, as well.
While compelling evidence is lacking, other alternative approaches may also improve recovery from stroke. These include:
Mind-body medicine may also help improve mindset and thus aid in recovery. These kinds of therapy include:
Tai chi
Meditation
Guided imagery
Relaxation
Qi gong
Some traditional medicines have been used to prevent or improve stroke complications. The active components in these herbs are not always known. Doses are also not regulated; therefore, standardized dosing is hard to establish. Speaking with a health care professional before taking any herbal medicines is best. Some herbal medicines that may benefit stroke survivors include:
Ginseng: This anti-inflammatory reduces oxidative stress but is best avoided by those taking blood thinners.
Red sage: Red sage should not be taken with blood thinners and may also interfere with certain heart medications.
Astragalus: This herb may help maintain the integrity of the blood-brain barrier.
Ashwagandha: Ashwagandha reduces inflammation and improves memory.
Gotu kola: Centella asiatica enhances memory and has been shown to improve cognitive function in stroke patients.
Ginkgo biloba: This well-studied botanical may improve neurological function. Avoid taking Gingko biloba if you’re on blood thinners.
Rosemary: The well-known herb has antioxidant properties and may reduce brain edema.
The results of the studies that have been done on these botanicals are promising, but more research is needed to support their use in treating strokes.
How Can I Prevent a Stroke?
About 4 in 5 strokes are preventable. You can also take steps to prevent recurrence and disability caused by stroke, though none of these is guaranteed.
A critical factor in preventing stroke is choosing a healthy lifestyle. Recommendations for adopting a healthy lifestyle include:
Managing high blood pressure: Follow your doctor’s prescription for any hypertension medications, and watch your sodium intake by avoiding processed foods.
Managing cholesterol: Avoid trans fats and take any required cholesterol medications.
Eating enough fiber: A high-fiber diet can help lower cholesterol.
Quitting smoking: If you smoke, talk to your health care provider about smoking cessation options.
Treating diabetes: Keep blood sugars within a healthy range by following a proper diet, exercising, and taking necessary medication.
Eating produce: Get five or more servings daily of fruits or vegetables.
Exercising regularly: Include aerobic exercises such as walking, jogging, bicycling, or swimming in your routine.
Watching your alcohol consumption: Having more than two drinks a day increases your stroke risk.
Treating obstructive sleep apnea: a sleep study may be recommended; wear a mask at night if prescribed.
Avoiding illegal drugs: Some may increase the risk of stroke.
Treating atrial fibrillation: Atrial fibrillation has an almost five-fold increase in stroke risk.
Medications can also help with stroke prevention if lifestyle changes are not enough. People with risk factors that can be managed by medication may be prescribed these drugs. These medications are:
Anti-platelet drugs: These drugs decrease platelet formation in the blood and make it less likely to clot. Some anti-platelet drugs are clopidogrel, prasugrel, and ticagrelor.
Anticoagulants: Commonly called blood thinners, drugs such as rivaroxaban, dabigatran, apixaban, and edoxaban reduce blood clotting.
The anticoagulants mentioned are newer and shorter-acting. Because of this, they usually do not require weekly blood tests and have a lower risk of bleeding complications, unlike their longer-acting counterparts.
Though these newer anticoagulants have benefits, there are situations where warfarin, a longer-acting anticoagulant, may be the better option. The National Institute on Neurological Disorders and Stroke suggests that warfarin is best for those with atrial fibrillation, those over the age of 65, or people with additional risk factors. Younger people with atrial fibrillation may have adequate protection from daily doses of aspirin.
Medically reviewed by Beverly Timerding, MD.
What topics would you like to read about? Please let us know at health@epochtimes.nyc