In this series, “Promise or Peril: Alarming COVID-19 mRNA Vaccine Issues,” we explore how the introduction of mRNA technology lacked an adequate regulatory framework, setting the stage for serious adverse events and other concerns related to inadequate safety testing of lipid nanoparticles, spike protein, and residual DNA and lipid-related impurities, as well as truncated/modified mRNA species.
Previously: We introduced how the FDA relaxed the rules for mRNA vaccines compared to mRNA therapies. We also discussed the available data for LNP distribution throughout the body based on animal testing and the fact that human testing was not done. Finally, we discussed the lack of biodistribution data on the mRNA and its encoded spike protein contained in the COVID mRNA vaccine.
We will now discuss how the LNPs are constructed and how they behave in the body. The engineering of these molecules must keep the capsule stable during transit but also allow it to dissolve quickly once injected.
If the LNPs are too stable, they may move throughout the body to distant organs instead of disintegrating locally at the injection site as intended. Other properties of the LNPs also affect the likelihood of adverse events, such as their electrical charge and their tendency to cluster.
Summary of Key Facts:
The lipid nanoparticle (LNP) capsule contains the active ingredient messenger RNA (mRNA).
The LNP is formed by lipids “teaming up” together to form a ball.
LNP molecules offer great potential as a delivery vehicle, however, the design of the LNP can cause harm.
The LNP capsule can cluster with other LNPs or fall apart after injection, potentially causing clotting.
If the LNP capsule falls apart, loose strands of mRNA can circulate in the blood.
Because the mRNA is negatively charged, loose mRNA in the blood can cause clotting if it clusters with positively charged molecules.
The LNP capsule lipids also have properties that may cause clotting or trigger the immune system to overreact.
Researchers knew about these possibilities before the vaccines were authorized.
The regulatory agencies knew about the possibility of harmful effects before they were even injected into the body.
The possibility of multiple boosters causing harm was also known before authorization.
As time passes, we are learning more about the possible mechanisms behind these adverse events.
The Food and Drug Administration (FDA) and European Medicines Agency (EMA) authorized a novel vaccine product based on laboratory studies and animal models, then applied these findings to humans. In addition, most of the mRNA research prior to the pandemic used intravenous (IV) injection directly into the bloodstream, not intramuscular (IM), as vaccines are typically delivered.
Various design challenges had to be overcome to create a vaccine built on a repurposed cancer-fighting platform, but some of these useful features of the LNP may be the flaws potentially contributing to adverse events.
LNP Design Features
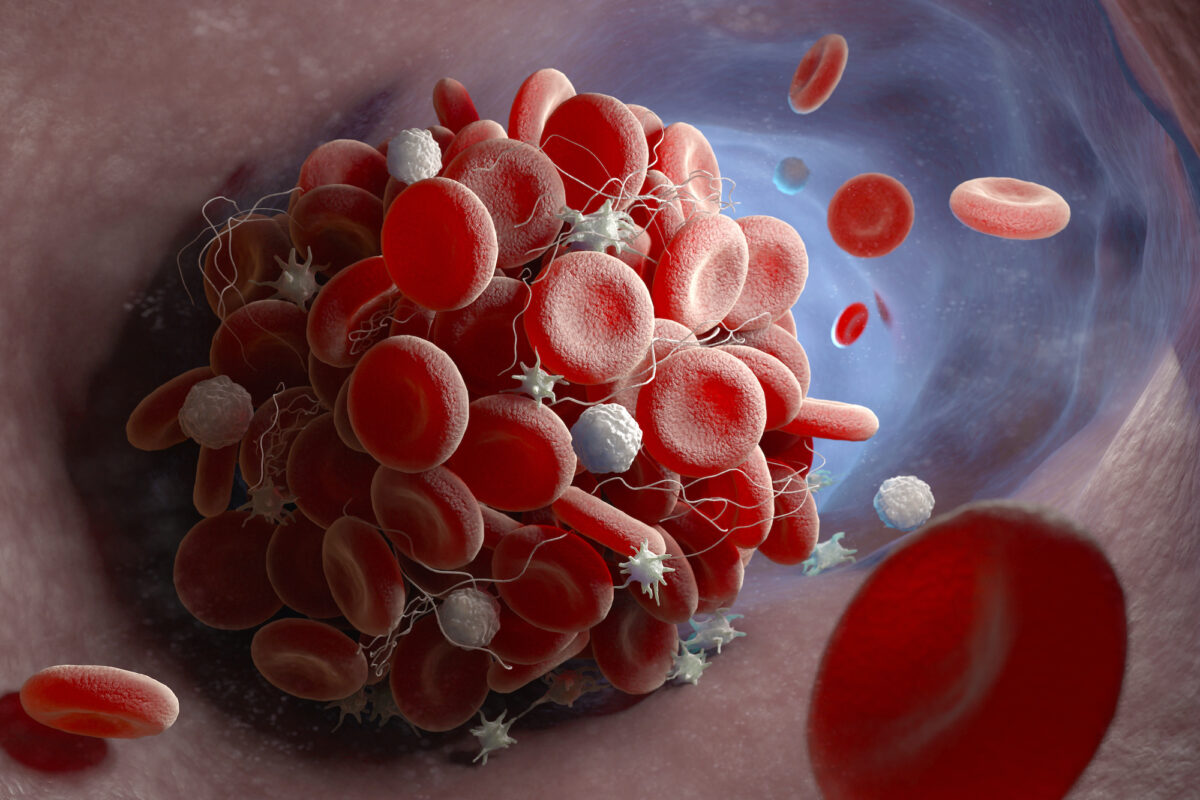
The LNP is a capsule comprised of four different lipids carrying the mRNA inside.
Imagine a drop of oil descending into a glass of water. The oil does not disperse in the water—it stays together. This is how the LNPs stay together to carry the mRNA to a cell membrane where it can be absorbed.
Certain features of the lipids cause them to organize into the LNP capsule shape. The tail of the lipid is hydrophobic, meaning it does not mix with water because it has a neutral charge. The head of the lipid is a phosphate that has an electrical charge, making it hydrophilic. These features cause them to organize themselves.
The lipids gather together—tails pointing in and heads pointing out—creating a ball, as pictured below. When the polyethylene glycol (PEG) adheres to a lipid, the PEG-lipid helps to stabilize the molecule, encouraging it to form smaller LNPs and preventing it from adhering to proteins in the blood.
In the center of the LNP is the RNA, which has a negative charge. When you add up the negative charge of the RNA and the positive charge of the phosphate heads on the lipids, the LNP net charge is mostly neutral, if not slightly negative.
Lipid nanoparticle mRNA vaccine, a type of vaccine used against COVID-19 and influenza. 3D illustration showing cross-section of a lipid nanoparticle carrying mRNA of the virus (orange).(Kateryna Kon/Shutterstock)
The PEG-lipids help keep the LNP from breaking apart. Once inside the cell, however, the LNP needs to split open to release the mRNA cargo. The cone-shaped configuration of the LNP can help this process.
The amount of PEG-lipids can affect particle size and zeta potential. Zeta potential is the electrical charge that develops around the surface of a particle. The zeta potential is important because it determines whether the LNPs tend to disperse or clump together. A high zeta potential—positive or negative—helps the nanoparticles disperse and float freely.
In addition, certain other PEG modifications affect how fast the kidneys and immune system clear the LNPs. If it takes a long time to clear the LNPs, they can circulate longer in the blood and create the potential for adverse events.
LNP Design Dilemmas: Stability Versus Fragility
The LNP design dilemma had serious implications: whether to create a stable LNP capsule that does not fall apart readily or a more fragile capsule that breaks down quickly. This design challenge affects how the capsule behaves in the body.
A highly stable capsule is useful for mRNA gene therapy, which is how this technology was originally developed. For gene therapy, the mRNA needs to be stable enough to reach its intended target and either produce a missing protein or turn off a harmful gene.
For vaccination, however, the opposite effect is desired: the LNP needs to be less stable so it will dissolve quickly at the injection site and release the fragile mRNA immediately. Otherwise, it will allow the LNP to travel throughout the human body to an unintended organ or tissue.
The biodistribution studies covered in Parts 1 and 2 tell us that the LNP mRNA design failed this “dual mission impossible.” Dispersion to distant organs peaked within about 48 hours. The effect of expressing spike protein on cells in these organs in humans is unknown, so simply adopting LNPs designed for gene therapy for direct usage in mRNA vaccine delivery will likely prove to be a significant mistake.
LNP Design Features Affect Clotting
In addition to the challenge of creating a stable LNP that breaks down quickly at the injection site, the LNP design may also cause clustering leading to clotting. If the LNP falls apart, the charges on the lipids and the loose mRNA may promote interactions with other substances in the blood.
These two factors may explain the potential for “thromboembolic” events. Thrombotic events involve the formation of a clot (thrombosis) in the bloodstream. Formation of the clot itself or its movement to another site (embolism) may block the flow of blood.
LNPs Can Cluster and Cause Clotting
When the LNPs diffuse into the blood system, the tiny particles can increase in size based on the Ostwald ripening phenomenon. This is a process in which small crystals dissolve in solution and then redeposit, forming larger clusters.
The diameter of arterioles, small blood vessels connecting arteries and capillaries, varies from 8000 to 60,000 nanometers (nm). A typical COVID-19 mRNA vaccine LNP is 60 to 200 nm. If the size of the clustered mRNA LNP particles increases to 5000 nm and above, LNPs could block blood vessels and cut off blood flow.
When thromboses occur within blood vessels, blood flow to critical organs can be obstructed. This includes the heart, lungs, kidneys, intestines, and even the brain.
For example, an autopsy review of 25 unexpected deaths that occurred within 20 days of COVID-19 vaccination found eight cases of thrombotic events, including five with “myocardial infarction,” two with “pulmonary embolism,” and one with “deep vein thrombosis.” (pdf)
Have human studies been conducted to assess the degree to which the LNPs cluster? To our knowledge, nothing has been published.
The LNP Can Fall Apart
If the LNP falls apart, two components, the capsule and the mRNA cargo, may cause interactions that promote clotting due to the electrical charge on each component.
The charge controls where the particles travel in the body. For instance, a positively charged LNP capsule can target the lung; a negatively charged LNP can target the spleen; while an LNP with an intermediate charge (such as mRNA COVID-19 vaccines) has a greater tendency to travel to the liver, as was seen in the preclinical biodistribution studies.
The potential for negatively charged free mRNA to cause problems was also seen with the adenovirus vector vaccines made by Astra-Zeneca and Johnson & Johnson, which caused blood clots in some people with a genetic predisposition.
Similarly, if the negatively charged mRNA slips out of the LNP carrier, it could theoretically lead to clotting due to its negative charge.
Could the challenges of maintaining a strict “cold chain” (freezing temperature required for vaccine stabilization from manufacturing to injection) have introduced the potential for LNPs to fall apart prior to injection?
“When the LNPs are frozen and thawed,” according to biotechnology consultant Christie Grace, “the [mRNA] can slip out, charges can start interacting with the human body and [potentially] cause clots.”
Dr. Ko, a South Korean professor of pharmacy who has written dozens of articles on LNPs, agrees that the molecules can break down and separate if pH and temperature are not carefully controlled.
What happens if the LNPs disintegrate in the vial before injection? What testing has been done to evaluate exposed mRNA (not lipid nanoparticle encapsulated mRNA) interactions in the blood?
LNP Engineering Can Alter Clotting
Nanoparticle interactions can be helpful or harmful. For example, nanoparticles can be engineered to help the blood to clot, which is useful for those with clotting disorders. On the other hand, if LNP interactions with other substances in the blood cause clotting, this is harmful.
What was known about the potential of LNPs to affect clotting before the pandemic?
In 2020, Faizullin, et al. reported: “We observed pronounced changes in both clot morphology and kinetics of fibrin clotting in the presence of artificial liposomes.” In other words, previous research on LNPs noted that clots looked different and fibrin behaved differently with LNPs.
Fibrin is a part of the human body’s natural clotting cascade. Binding to fibrin accelerates the normal clotting process. Faster fibrin clotting has been observed in laboratory studies using blood from patients with COVID-19. This clotting tendency may be due to the presence of the spike protein’s S1 subunit. Thus, the LNP mRNA vaccine may promote clotting either due to the design of the LNP, the presence of the spike protein’s S1 subunit, or both.
‘Immune Overdrive’
Finally, the mRNA was engineered to help it sneak past our natural immune defenses. This clever design feature may have a fatal flaw.
Our immune system looks for special patterns to detect invading microbes. One of these patterns is foreign RNA. To avoid being detected before the vaccine has a chance to work, one part of the COVID-19 vaccine mRNA—uridine—was replaced with pseudouridine.
However, if the immune system never notices, then we do not get the intended benefit. Adjuvants, such as aluminum, are added to vaccines for this reason—to wake up the immune system. Once stimulated, the immune system ramps up its production of antibodies and memory T cells.
The lipids used to create the LNP capsule may also stimulate the immune system via the same pattern detectors used to find harmful invaders. Although this may make them an effective adjuvant for the vaccine, mouse models suggest that LNPs may put the immune system into “overdrive.”
The EMA noted in its report that the innate immune system ramps up immediately after injection, peaks at six hours, then returns to baseline nine days later. An article in Cell also discussed the innate immune system in the context of vaccine adverse events (AEs). The authors noted that “frequent booster immunizations may increase the frequency and/or the severity of the reported AEs.”
What Was Known Prior to Authorization?
Early research on LNPs suggests the following issues were well-documented before the COVID-19 vaccines were authorized:
1) Off-target travel throughout the body is determined by the charge of the LNP.
2) The innate immune system is triggered by LNPs that could run the risk of causing an over-reaction.
3) The cationic (negatively charged) lipid particles are linked to immune stimulation.
4) The mode of delivery matters (via muscle or bloodstream), affecting where the LNPs travel.
5) The LNPs were specifically designed for the uptake by the lymphatic system, as discussed in a previous Epoch Times article.
These effects were known prior to FDA authorization and strongly suggest that more testing should have been done in humans.
Carrasco et al. appears to agree with our concerns about the need to better understand biodistribution in humans. They noted that “A specific and important application of these new insights is in the reduction of systemic distribution and off-target expression after IM vaccine delivery.”
Knowledge about charged particle trafficking throughout the body is limited and primarily based on intravenous (IV) injections; only one study published prior to the pandemic explored how an intramuscular injection would affect LNP dispersion.
A 2021 Nature article sums up the importance of careful design. They note, as did the EMA, that negatively charged LNPs concentrate in the liver following injection. “This undesirable systemic off-target expression of mRNA-LNP vaccines could be minimized through appropriate design of the ionizable lipid and LNP.”
Pulling back the curtain on the LNP design, we see that several features intended for stealth delivery of mRNA to the cell have set the stage for a wide range of adverse events which should have been anticipated through testing, and prevented through cautious policy.
Read Part 1: FDA Overhaul Needed for New Vaccines and mRNA Therapies
Read Part 2: Health Implications of Poor COVID-19 mRNA Testing: Miscarriage, Vision Loss, Immunotoxicity
Next: In Part 4 we turn to the cargo contained within the LNP capsule—the mRNA and its encoded spike protein. We also drill down into how the spike protein and its S1 subunit might impact the cardiovascular system, and how recent research suggests that an over-active natural response (cytokines) may cause myocarditis. While the FDA has acknowledged that passive surveillance is not enough to study the adverse events, its required postmarketing study is now more than six months overdue.
◊References
Addgene. Molecular Biology Reference. https://www.addgene.org/mol-bio-reference/#introduction
Alana F Ogata, Chi-An Cheng, Michaël Desjardins, Yasmeen Senussi, Amy C Sherman, Megan Powell, Lewis Novack, Salena Von, Xiaofang Li, Lindsey R Baden, David R Walt, Circulating Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Vaccine Antigen Detected in the Plasma of mRNA-1273 Vaccine Recipients, Clinical Infectious Diseases, Volume 74, Issue 4, 15 February 2022, Pages 715–718, https://doi.org/10.1093/cid/ciab465
Aldén M, Olofsson Falla F, Yang D, Barghouth M, Luan C, Rasmussen M, De Marinis Y. Intracellular Reverse Transcription of Pfizer BioNTech COVID-19 mRNA Vaccine BNT162b2 In Vitro in Human Liver Cell Line. Curr Issues Mol Biol. 2022 Feb 25;44(3):1115-1126. doi: 10.3390/cimb44030073. PMID: 35723296; PMCID: PMC8946961. https://pubmed.ncbi.nlm.nih.gov/35723296/
Anderson EJ, Rouphael NG, Widge AT, et al. Safety and Immunogenicity of SARS-CoV-2 mRNA-1273 Vaccine in Older Adults N Engl J Med 2020; 383:2427-2438 https://www.nejm.org/doi/full/10.1056/NEJMoa2028436
Anderson S. CBER Plans for Monitoring COVID-19 Vaccine Safety and Effectiveness. https://stacks.cdc.gov/view/cdc/97349 October 20, 2020. Accessed 3/20/23.
Angeli F, Spanevello A, Reboldi G, Visca D, Verdecchia P. SARS-CoV-2 vaccines: Lights and shadows. Eur J Intern Med. 2021 Jun;88:1-8. doi: 10.1016/j.ejim.2021.04.019. Epub 2021 Apr 30. PMID: 33966930; PMCID: PMC8084611. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8084611/#bib0043
Baker, A. T., Boyd, R. J., Sarkar, D., Teijeira-Crespo, A., Chan, C. K., Bates, E., Waraich, K., Vant, J., Wilson, E., Truong, C. D., Lipka-Lloyd, M., Fromme, P., Vermaas, J., Williams, D., Machiesky, L., Heurich, M., Nagalo, B. M., Coughlan, L., Umlauf, S., Chiu, P. L., … Borad, M. J. (2021). ChAdOx1 interacts with CAR and PF4 with implications for thrombosis with thrombocytopenia syndrome. Science Advances. 7(49), eabl8213. https://doi.org/10.1126/sciadv.abl8213
Baumeier C, Aleshcheva G, Harms D, Gross U, Hamm C, Assmus B, Westenfeld R, Kelm M, Rammos S, Wenzel P, Münzel T, Elsässer A, Gailani M, Perings C, Bourakkadi A, Flesch M, Kempf T, Bauersachs J, Escher F, Schultheiss H-P. Intramyocardial Inflammation after COVID-19 Vaccination: An Endomyocardial Biopsy-Proven Case Series. International Journal of Molecular Sciences. 2022; 23(13):6940. https://doi.org/10.3390/ijms23136940
Bloom, K., van den Berg, F. & Arbuthnot, P. Self-amplifying RNA vaccines for infectious diseases. Gene Ther 28, 117–129 (2021). https://doi.org/10.1038/s41434-020-00204-y. https://www.nature.com/articles/s41434-020-00204-y (only need one link)
Carrasco, M.J., Alishetty, S., Alameh, MG. et al. Ionization and structural properties of mRNA lipid nanoparticles influence expression in intramuscular and intravascular administration. Commun Biol 4, 956 (2021). https://doi.org/10.1038/s42003-021-02441-2
Chauhan, H., Mohapatra, S., Munt, D.J. et al. Physical-Chemical Characterization and Formulation Considerations for Solid Lipid Nanoparticles. AAPS PharmSciTech 17, 640–651 (2016). https://doi.org/10.1208/s12249-015-0394-x
Chui CSL, Fan M, Wan EYF, et al. Thromboembolic events and hemorrhagic stroke after mRNA (BNT162b2) and inactivated (CoronaVac) covid-19 vaccination: A self-controlled case series study. Lancet. 2022;(50). https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00234-6/fulltext
Dag Berild J, Bergstad Larsen V, Myrup Thiesson E, et al. Analysis of Thromboembolic and Thrombocytopenic Events After the AZD1222, BNT162b2, and MRNA-1273 COVID-19 Vaccines in 3 Nordic Countries. JAMA Netw Open. 2022;5(6):e2217375. doi:10.1001/jamanetworkopen.2022.17375 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2793348
daSilva RL. Viral-associated thrombotic microangiopathies. Hematology/Oncology and Stem Cell Therapy. 2011:4(2):51-59. https://www.sciencedirect.com/science/article/pii/S165838761150038X
De A, Ko YT. Why mRNA-ionizable LNPs formulations are so short-lived: causes and way-out. Expert Opin Drug Deliv. 2023 Feb;20(2):175-187. doi: 10.1080/17425247.2023.2162876. Epub 2023 Jan 1. PMID: 36588456. https://pubmed.ncbi.nlm.nih.gov/36588456/
Ehaideb, S.N., Abdullah, M.L., Abuyassin, B. et al. Evidence of a wide gap between COVID-19 in humans and animal models: a systematic review. Crit Care 24, 594 (2020). https://doi.org/10.1186/s13054-020-03304-8
European Medicines Agency https://www.ema.europa.eu/en/documents/assessment-report/comirnaty-epar-public-assessment-report_en.pdf
Faizullin D, Valiullina Y, Salnikov V, Zuev Y. Direct interaction of fibrinogen with lipid microparticles modulates clotting kinetics and clot structure. Nanomedicine. 2020 Jan;23:102098. doi: 10.1016/j.nano.2019.102098. Epub 2019 Oct 23. PMID: 31655206. https://pubmed.ncbi.nlm.nih.gov/31655206/
FDA. Considerations for Human Radiolabeled Mass Balance Studies – Guidance for Industry. https://www.fda.gov/media/158178/download May, 2022.
FDA. Development and Licensure of Vaccines to Prevent COVID-19. https://www.fda.gov/media/139638/download
FDA-CBER-2021-5683-0013962 approved on: 09-Nov-2020. A Tissue Distribution Study of a [3H]-Labeled Lipid Nanoparticle-mRNA Formulation Containing ALC-0315 and ALC-0159 Following Intramuscular Administration in Wistar Han Rats. FINAL REPORT Test Facility Study No. 185350 Sponsor Reference No. ALC-NC-0552 https://phmpt.org/wp-content/uploads/2022/03/125742_S1_M4_4223_185350.pdf
Fertig TE, Chitoiu L, Marta DS, Ionescu VS, Cismasiu VB, Radu E, Angheluta G, Dobre M, Serbanescu A, Hinescu ME, Gherghiceanu M. Vaccine mRNA Can Be Detected in Blood at 15 Days Post-Vaccination. Biomedicines. 2022 Jun 28;10(7):1538. doi: 10.3390/biomedicines10071538. PMID: 35884842; PMCID: PMC9313234. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9313234/
Grobbelaar LM et al. SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: implications for microclot formation in COVID-19 Biosci Rep (2021) 41 (8): BSR20210611. https://doi.org/10.1042/BSR20210611
Hassett, KJ, Benenato KE, Jacquinet E, et al. Optimization of Lipid Nanoparticles for Intramuscular Administration of mRNA Vaccines. Molecular Therapy: Nucleic Acids. 2019;15:P1-11. https://doi.org/10.1016/j.omtn.2019.01.013
Hou, X., Zaks, T., Langer, R. et al. Lipid nanoparticles for mRNA delivery. Nat Rev Mater 6, 1078–1094 (2021). https://doi.org/10.1038/s41578-021-00358-0
Let’s talk about lipid nanoparticles. Nat Rev Mater 6, 99 (2021). https://www.nature.com/articles/s41578-021-00281-4
Michieletto, D., Lusic, M., Marenduzzo, D. et al. Physical principles of retroviral integration in the human genome. Nat Commun 10, 575 (2019). https://doi.org/10.1038/s41467-019-08333-8
Moghimi, S. M., & Simberg, D. (2022). Pro-inflammatory concerns with lipid nanoparticles. Molecular therapy : The Journal of the American Society of Gene Therapy, 30(6), 2109–2110. https://doi.org/10.1016/j.ymthe.2022.04.011
Naturally Inspired Podcast. Jessica Rose PhD – VAERS, Data And Truth https://www.audible.com/pd/Jessica-Rose-PhD-VAERS-Data-And-Truth-Podcast/B09YMLJGBN?clientContext=132-5166709-6339436&loginAttempt=true&noChallengeShown=true
Ohlson J. Plasmid manufacture is the bottleneck of the genetic medicine revolution. Drug Discov Today. 2020 Oct 16;25(11):1891–3. doi: 10.1016/j.drudis.2020.09.040. Epub ahead of print. PMID: 33075470; PMCID: PMC7564888. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7564888/
Perico L, Marina Morigi M, Galbusera M, et al. SARS-CoV-2 Spike Protein 1 Activates Microvascular Endothelial Cells and Complement System Leading to Platelet Aggregation. Front. Immunol. 2022 https://www.frontiersin.org/articles/10.3389/fimmu.2022.827146/full
Qin, S., Tang, X., Chen, Y. et al. mRNA-based therapeutics: powerful and versatile tools to combat diseases. Sig Transduct Target Ther 7, 166 (2022). https://doi.org/10.1038/s41392-022-01007-w
Röltgen K, Nielsen SCA, Silva O. Immune imprinting, breadth of variant recognition, and germinal center response in human SARS-CoV-2 infection and vaccination. Cell 2022;185(6):1025-1040. https://www.cell.com/cell/fulltext/S0092-8674(22)00076-9
Schmeling, M, Manniche, V, Hansen, PR. Batch-dependent safety of the BNT162b2 mRNA COVID-19 vaccine. Eur J Clin Invest. 2023; 00:e13998. doi:10.1111/eci.13998 https://pubmed.ncbi.nlm.nih.gov/36997290/
Srinivasan M, Thangaraj SR, Arzoun H. Gene Therapy – Can it Cure Type 1 Diabetes? Cureus. 2021 Dec 19;13(12):e20516. doi: 10.7759/cureus.20516. PMID: 35004071; PMCID: PMC8723777. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8723777/
Trevaskis, N., Kaminskas, L. & Porter, C. From sewer to saviour — targeting the lymphatic system to promote drug exposure and activity. Nat Rev Drug Discov 14, 781–803 (2015). https://doi.org/10.1038/nrd4608
Trougakos IP, Terpos E, Alexopoulos H, et al. Adverse effects of COVID-19 mRNA vaccines: the spike hypothesis. Cell 2022;28(7): P542-554. https://www.cell.com/trends/molecular-medicine/fulltext/S1471-4914(22)00103-4
Vervaeke P, Borgos SE, Sanders NN, Combes F. Regulatory guidelines and preclinical tools to study the biodistribution of RNA therapeutics. Adv Drug Deliv Rev. 2022 May;184:114236. doi: 10.1016/j.addr.2022.114236. Epub 2022 Mar 26. PMID: 35351470; PMCID: PMC8957368. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8957368/
Wong DWL, Klinkhammer BM, Djudjaj S, Villwock S, Timm MC, Buhl EM, Wucherpfennig S, Cacchi C, Braunschweig T, Knüchel-Clarke R, Jonigk D, Werlein C, Bülow RD, Dahl E, von Stillfried S, Boor P. Multisystemic Cellular Tropism of SARS-CoV-2 in Autopsies of COVID-19 Patients. Cells. 2021 Jul 27;10(8):1900. doi: 10.3390/cells10081900. PMID: 34440669; PMCID: PMC8394956. https://pubmed.ncbi.nlm.nih.gov/34440669/
Yonker LM, Swank Z, Bartsch YC, et al. Circulating Spike Protein Detected in Post–COVID-19 mRNA Vaccine Myocarditis. Circulation. 2023:147(11). https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.122.061025