The topic of “leaky gut” has gained increasing attention in recent years. Some believe that it is the cause of many diseases, while others do not think the disease exists.
‘Leaky Gut’ Is Not a Medical Term, but It Exists
“Leaky gut” is a layman’s term, and it does not correspond to a medical diagnosis; medically, it refers to increased intestinal permeability or gut-barrier loss.
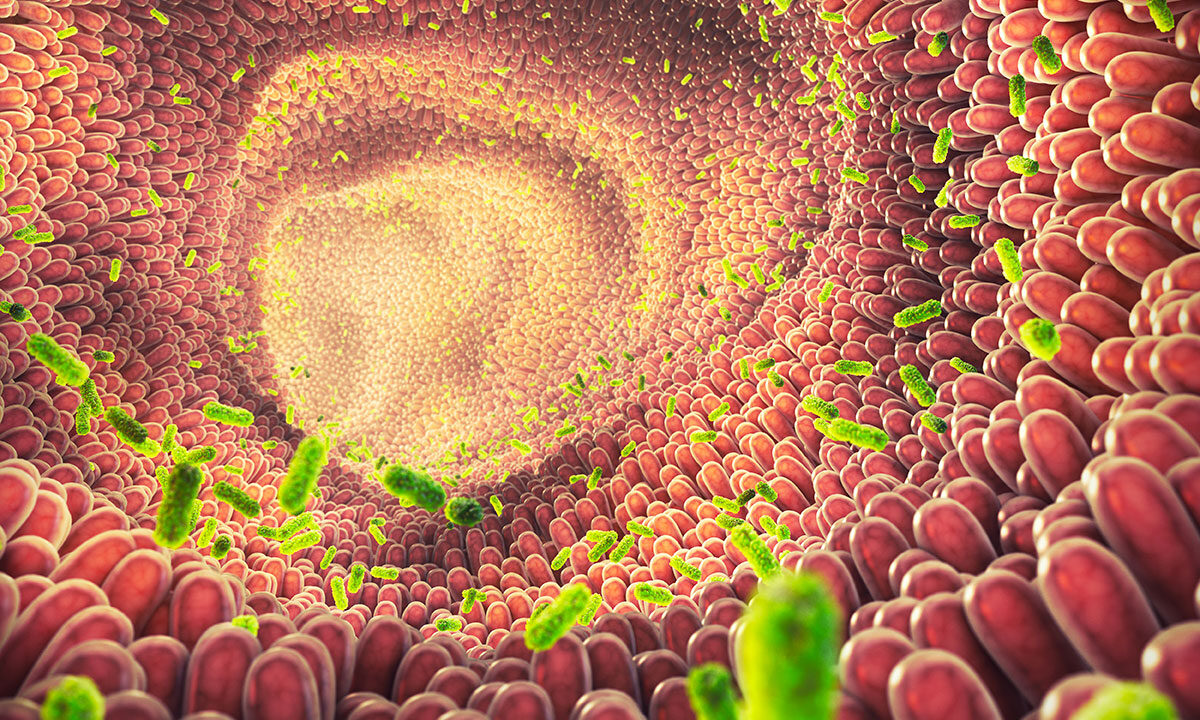
The gut barrier is a key immune barrier in the human body, consisting of a layer of intestinal epithelial cells and a mucus layer. The human intestinal epithelium covers a surface area of up to 400 square meters. Intestinal epithelial cells are linked together by tight junction proteins. They keep substances in the gut lumen, including pathogens (viruses and bacteria) and food debris, from entering the bloodstream.
If the seal between the epithelial cells of the intestinal tract is reduced, like a door that is not closed tightly and has a gap, the bacteria and toxins in the gut lumen will “leak.” This can trigger various adverse reactions, such as inflammation and some chronic diseases.
In addition, there is another type of leaky gut. Instead of passing through the gaps between the intestinal epithelial cells, some toxic substances destroy and penetrate the intestinal epithelial cells, and enter the human body directly.
Differences between a healthy intestinal epithelium and a “leaky gut” epithelium. (The Epoch Times)
Intestinal permeability is objective and measurable.
The lactulose:mannitol test is one of the more common methods, in which the subject will drink a reagent containing lactulose and mannitol. Lactulose cannot be directly absorbed by cells; the only way it can be absorbed by the human body is through the gap between intestinal epithelial cells and into the bloodstream, and eventually excreted in urine, while mannitol can be directly absorbed by cells. Intestinal permeability can be calculated to some extent by measuring the levels and ratios of these two substances in the urine.
The intestinal epithelial cells are tightly connected, but not entirely impregnable.
In fact, the intestinal tract must maintain a certain level of permeability, as it is important for our health. For example, sodium and water need to be able to cross the intestinal barrier. Experiments have shown loss of this selective permeability, or leakiness, for sodium and water results in malnutrition and death in mice study, Jerrold Turner, a professor of pathology and medicine at Harvard Medical School and Brigham and Women’s Hospital said in an interview with The Epoch Times.
Many Chronic Diseases Are Accompanied by Leaky Gut Problems
It has been found experimentally and clinically that patients with the following diseases tend to have increased gut permeability:
Inflammatory bowel disease (IBD)
Irritable bowel syndrome (IBS)
Type 1 and Type 2 diabetes
Depression
Alcoholic liver disease
Nonalcoholic steatohepatitis (NASH)
Liver cirrhosis
Severe acute pancreatitis (SAP)
Primary biliary cholangitis (PBC)
There are also some other diseases and syndromes that are thought to be associated with intestinal barrier dysfunction, such as autism, eczema, psoriasis, Parkinson’s disease, fibromyalgia, chronic fatigue syndrome, asthma, multiple sclerosis, etc.
Despite this, it is difficult to determine if gut permeability increase will cause disease, the disease causes increased gut permeability, or the two are independent events. In part, this is because available human data are limited to correlation, which cannot be used to establish causality, said Turner.
Leaky Gut and IBS, A Closer Look
Turner told The Epoch Times that the best evidence linking increased permeability, or barrier loss, to disease is in the context of Crohn’s disease, a form of inflammatory bowel disease (IBD).
Nearly 40 years ago, doctors at the University of California, Los Angeles, and the University of California, Irvine, studied relatives of Crohn’s disease patients. Even though these people were healthy, a small number of them have increased permeability.
In 2020, doctors at Mount Sinai Hospital in Toronto, Canada, published another study. They followed healthy relatives of Crohn’s disease patients for up to 7.8 years after a single permeability test. They compared outcomes of these relatives with increased permeability to those with normal permeability and found that increased permeability was associated with a greater risk of developing IBD.
Turner noted, despite this, that most of the relatives, including those with increased permeability, did not develop IBD. This suggests that increased gut permeability only causes disease when combined with other defects, such as immune activation.
Other groups of researchers have studied patients with Crohn’s disease during clinical remission. They found that increased permeability was predictive of relapse. (1, 2, 3)
Studies of mice that have increased intestinal permeability support this idea. The mice were healthy and grew normally. However, when challenged with disease-inducing stimuli, mice with increased intestinal permeability developed more severe disease than their siblings’ normal permeability. (1, 2, 3)
Even in the absence of these stressors, the mice with increased intestinal permeability had mild mucosal immune activation, perhaps to compensate for increased gut permeability. (1, 2)
Data Showing Causality Are ‘Beginning to Emerge’
More recently, Turner’s group discovered that these mice also displayed anxiety-like behaviors. In this model, immune activation and behavioral changes were caused by increased permeability.
Thus, although much more study is needed, “data showing that barrier loss can cause abnormalities are beginning to emerge,” said Turner.
Can Leaky Gut Be Treated?
“There may be approaches to treat barrier loss in the foreseeable future,” Turner said. However, “for now, there are no therapies that can directly restore the gut barrier.”
As for whether treating gut permeability can improve the associated diseases, scientists still haven’t got a conclusion.
An effective treatment to restore the intestinal barrier is needed before clinical trials are possible, said Turner. Without effective treatment, scientists cannot do clinical trials on patients to see if restoring the gut barrier can be of benefit to patients with chronic diseases, including IBD, graft-versus-host disease, diabetes, liver disease, and others. (1, 2, 3)
Yet Turner did a mice study and found that preventing increased gut permeability can limit experimental IBD and graft-versus-host disease, a complication of bone marrow transplantation.
He has also developed drug-like molecules that can restore the barrier and prevent experimental IBD.
These molecules are not safe for people, but they are being used as tools to develop similar agents that may be used to treat or prevent disease in patients and individuals at risk of developing disease, he said.
It is also important to remember that there are multiple reasons for the intestinal barrier to be damaged. In addition to having treatments, it will be critical to be able to determine the processes that have caused increased gut permeability in any one patient, said Turner.
In a word, to understand the mystery of our gut, there’s a long way to go.
4 Ways to Improve Gut Lining Health
Scientists are continuing to investigate the benefits of various therapeutics for improving the health and integrity of the gut lining.
These therapies may not be able to mitigate a pathological disease, but they may help mitigate the effects of everyday factors such as diet, stress, and bacterial overgrowth that can wear on your intestinal lining. They may even help alleviate your general gastrointestinal symptoms.
Avoid Foods That Trigger Allergies
Studies have shown that people with food allergies usually have impaired intestinal barrier function. In the lactulose:mannitol test, people with food allergies show a value three times that of people without allergies, indicating that their intestinal permeability is higher.
Some people have intolerances to certain foods, but unlike a natural allergy, it is not lifelong. Dr. Michael Chang, the founder and attending physician of Healed and Whole Clinic, said in an interview with The Epoch Times that certain food intolerances are reversible. He would advise patients to avoid the food they cannot tolerate for at least half a year so that the intestines have a chance to repair and heal themselves; then try to gradually add the food back to the diet.
Eat Flavonoids and a Balanced Diet
Flavonoids have been proven to help improve the barrier function of the intestinal epithelium. They act on tight junction proteins to protect barrier integrity and also regulate the gut microbiota. Flavonoids are found in most vegetables, fruits, green and black teas, red wine, chocolate, and coffee. Consumption of cranberry extract for up to nine weeks increased the abundance of a beneficial bacterium in the gut by 30 percent, which is essential for protecting gut integrity.
A balanced diet complete with all the necessary macronutrients and micronutrients (vitamins and minerals) can help fortify your gut.
Vitamin D and an amino acid called L-glutamine may specifically help repair the gut lining. What’s more, prebiotics and probiotics could restore gut barrier function by preventing the overgrowth of the wrong bacteria and helping the good bacteria in your gut.
Avoid Processed Foods and Sugar
The widespread use of industrial food additives in modern society has also been linked to intestinal barrier dysfunction and the rising incidence of autoimmune diseases. Carboxymethylcellulose (CMC) and polysorbate are two of the most commonly used additives in the food industry. Experiments on animals have shown that they lead to a decrease in the thickness of intestinal mucus, which increases bacterial contact with intestinal epithelial cells and causes inflammation.
Additionally, the high-fat and high-sugar Western diet is also detrimental to the improvement of intestinal permeability. A high-fat and high-sugar diet can induce changes in gut microbiota composition, reduce the thickness and quality of the intestinal mucus layer, and increase intestinal permeability, thus increasing the occurrence of inflammation.
Avoid Prolonged Strenuous Exercise
Stress is a lifestyle factor that worsens gut-barrier function through interactions of the gut-brain axis. Scientists in Belgium conducted a study in which healthy volunteers were tested for cortisol levels in their saliva after public speaking, and the results showed that acute psychological stress increases intestinal permeability.
Moderate-intensity exercise can reduce stress, but the stress caused by strenuous and prolonged exercise is worth mentioning. Some athletes often experience abdominal discomfort; this is due to the release of stress hormones during strenuous exercise. Blood will flow from the gut and be redistributed throughout the body during intense or prolonged physical activity; elevated body temperature and changes in the gut microbiota will lead to the loosening of tight junction proteins and inflammatory responses. One study found that prolonged combat training increased intestinal permeability in soldiers.